“You mainly feel the way you think.” (Albert Ellis.)
The central principle that underpins CBT therapy is the concept that our thoughts and images (cognitions) influence our feelings (emotions); that this relationship creates changes in our bodies (physiological sensations) which in combination, determine our actions (behavioural responses.)
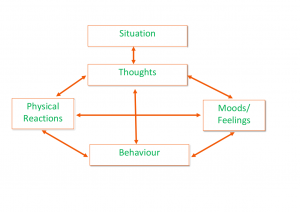
This ongoing cycle is fundamental to understanding all human behaviour. Where positive thoughts influence desirable emotions, welcomed physiological sensations and productive behaviour, by contrast, negative thoughts will influence undesirable emotions, unwanted physiological sensations and result in unproductive behaviour.
“Whatever a person frequently thinks and reflects on, that will become the inclination of their mind.” (Gautama Buddha.)
CBT therapy acknowledges that whilst we will all have experiences of helpful cycles; it is the unhelpful cycles that result in the development and ongoing maintenance of clinical symptoms associated with common emotional disorders.
By gaining mastery in any one of the areas associated with your cognitions, emotions, physiological sensations or behaviours, you can directly-influence the other areas of that cycle, which with repeated practice will enable you to achieve significant change.
The process of formulation:
“Always look at the function, it’s not what you did, but why. Once you find the why you walk through another door.” (Matt Broadway-Horner.)
A CBT treatment plan will always be guided by a joint understanding of your problems, developed between you and your therapist (whether that’s myself or another) that informs the focus, pace and delivery of therapy. This process is referred to as Formulation and is a process that develops over the course of treatment to provide a central framework to understand your problem(s), to identify changes and to equip you with coping skills for future self-management (referred to as relapse prevention.)
Three main aspects will always be considered as part of the formulation process. An understanding of the predisposing factors (usually informed from childhood) that may have left you vulnerable to the development of your current clinical symptoms; the precipitating factors (usually, life events and/or changes in your circumstances) that have served as a catalyst in the onset of your clinical symptoms; and the perpetuating factors (negative thoughts; undesirable emotions; unwanted physical sensations and unhelpful behavioural responses) that have been maintaining your ongoing clinical presentation.
An analogy that I frequently use to demonstrate the role that formulation will offer your treatment, is that of a jigsaw puzzle.
Imagine that you have a box with your name on it. Inside that box lie the pieces of a jigsaw puzzle; specifically, your jigsaw puzzle that depicts “you.” Your life, your experiences, your strengths, your areas of difficulty. All the things that have made you the person that you are today. Unlike most jigsaw puzzles, your box is missing the “big picture.” You are pretty sure that you have all the pieces, but without your “big picture” to work from, piecing them altogether might seem a confusing and possibly daunting task?
Formulation is the process that we use to help put your “big picture” together. Whether we start with your “corners” (representing clusters of the clinical symptoms that you are experiencing) or whether you’d prefer to “start-in-the-centre-and-work-outwards,” the combination of our therapeutic discussions with shared curiosity, guided discovery and your feedback from evidence gained through homework assignments will help us in gradually piecing it all together.

This completed big picture is essential, both for guiding treatment as well as promoting your ongoing wellbeing. It will provide you with your own personal template for understanding why your current problems came to develop and which unhelpful thoughts and behaviours may have been maintaining your problems. This information will then help you to make predictions about the particular themes and scenarios that you may be vulnerable to in the future. Armed with this new insight and the CBT strategies you learn in treatment, you will be able to recognise future triggers sooner and consciously-choose how to respond, reducing the likelihood and/or severity of clinical setbacks and maintaining change.
Clinical presentations CBT can help with:
The following list is by no-means exhaustive, but offers an overview of the range in presentations that CBT has been evidenced as an effective psychological treatment:
- Depression
- Anxiety Disorders, including:
- Health Anxiety,
- Obsessive Compulsive Disorder
- Phobias
- Social Anxiety
- Generalised Anxiety Disorder
- Panic Disorder
- Agoraphobia
- Post-Traumatic Stress Disorder
- Body Dysmorphic Disorder
- Clinical perfectionism
- Low self esteem
- Complicated grief reactions
- Eating Disorders
- Addictions
If you think that you might be experiencing clinical symptoms, please visit MIND’s website (www.mind.org.uk) for their full range of PDF booklets, via AZ mental health.
